How to prevent nocturnal hypoglycemia and optimize recovery

At Glucovibes, we have noticed the high frequency of nocturnal hypoglycemia, especially among people who engage in sports. Many of our users have asked about the relationship between nocturnal hypoglycemia and recovery, and how to prevent it. If you have experienced any nocturnal hypoglycemia (blood glucose <70 mg/dL) during the sensor trial phase and want to learn how to prevent nocturnal hypoglycemia and optimize recovery, keep reading!
What does nocturnal hypoglycemia suggest? Physiological meaning
Understanding the physiology of blood glucose (and if you don’t, we explain it very clearly here) will make it easy to grasp why nocturnal hypoglycemia occurs. In brief, maintaining blood glucose levels is a physiological priority because glucose is a crucial energy substrate for various cells in the body. A sharp decrease in glucose can lead to disorientation, seizures, and in severe cases, even death (1). The liver is the master organ in glucose regulation due to its significant capacity for glucose storage and secretion (2). Although muscle represents the largest glucose reservoir in absolute terms, it lacks the enzyme necessary for glucose to return to the bloodstream. Consequently, glucose stored in the muscle does not directly influence blood glucose levels.
Hypoglycemia is defined as a blood glucose concentration lower than 70 mg/dL, but what does this mean? Blood glucose levels represent the balance between glucose leaving the liver and entering peripheral tissues. Therefore, hypoglycemia occurs when glucose “output” is less than glucose “input” or when glucose “input” is increased. But why does hypoglycemia happen? The central nervous system (CNS) and red blood cells have a continuous glucose demand and lack the capacity to store glycogen. Thus, the glucose they use comes from blood glucose levels, which in turn, comes from the liver. If hepatic glycogen reserves are low before bedtime, they may become depleted, potentially leading to episodes of nocturnal hypoglycemia. In these cases, the body activates compensatory mechanisms to increase blood glucose and maintain proper functioning. These compensatory mechanisms include the secretion of the following hormones:
- Increased cortisol
- Increased GH (growth hormone)
- Increased glucagon
- Increased epinephrine (3).
As a result, blood glucose levels return to their normal range.
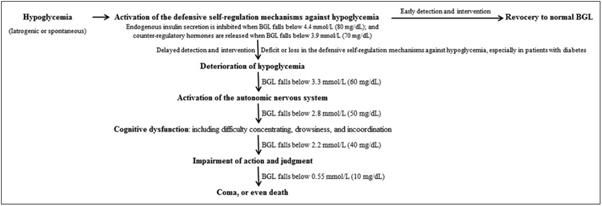
Our body prioritizes glucose supply to the brain over other organs (e.g., muscle), and when hypoglycemia is severe, it reduces glucose delivery to the brain, causing dizziness, fatigue, weakness, headaches, speech disturbances, etc. This is why prolonged and severe hypoglycemia can lead to irreversible brain damage. Regarding athletic performance, after analyzing various cases of athletes, we at Glucovibes have noticed that constant hypoglycemia can also result from elevated fatigue. This accumulated fatigue leads to persistent hypoglycemia, which in turn causes overactivation of the nervous system. As a result, cortisol levels (the stress hormone) may be elevated, often due to poor nutrition or insufficient recovery.
Why can it compromise recovery?
One of the main issues we encounter at Glucovibes is the low carbohydrate intake among endurance athletes. Given that the dependence on carbohydrates increases exponentially with exercise intensity (higher intensity means greater reliance on glucose), carbohydrates are essential for optimal performance and recovery.
💡 Carbohydrates are crucial for optimal performance and recovery.
As previously mentioned, frequent hypoglycemia can result from accumulated fatigue, indicating poor recovery.
Firstly, a low intake of carbohydrates (especially after exercise) is the primary cause of low glycogen levels. This, in turn, directly impacts athletic performance, as low glycogen levels are associated with decreased performance and increased fatigue. If carbohydrate intake (especially in the post-exercise period) is insufficient to replenish glycogen stores, your performance in the next training session will suffer, and your hormonal response to exercise stress will be greater. This prolonged situation can lead to significant fatigue accumulation. Consequently, frequent hypoglycemia occurs, creating a vicious cycle (poor recovery → frequent hypoglycemia → overactivation of the nervous system) which can be broken in two ways:
1. Consuming the correct amount of carbohydrates for your sport.
2. Properly resting and recovering between training sessions before starting the next one.

How to avoid nocturnal hypoglycemia and optimize recovery
To avoid nocturnal hypoglycemia and optimize recovery, it’s crucial to focus on the following:
- Post-Workout Nutrition and Pre-Bed Snack: The timing of your workout plays a role here, with greater importance if you train in the evening or night.
- Proper Rest: If your goal is related to athletic performance, this part will be very relevant, and an example should make it clear.
Imagine you’re training for the Ehunmilak (a 168 km mountain endurance race) and have completed a 3-hour workout from 6:00 PM to 9:00 PM. You get home feeling very hungry and decide to eat dinner before showering. For that dinner (your post-workout meal), it’s recommended to include an adequate amount of carbohydrates along with high-quality protein. For example, you could have a bowl of quinoa with vegetables as a starter and grilled chicken breast with a mixed salad as a main dish. After dinner, you shower and then decide to watch an episode of your favorite Netflix series. While watching, you could have a snack or dessert like natural yogurt with oats and banana, adding more carbohydrates.
The carbohydrates consumed will help replenish both liver and muscle glycogen, making it less likely that you’ll experience hypoglycemia during sleep, thereby optimizing your recovery.

In summary, it’s essential to have a broad understanding of how blood glucose is regulated and the key organ involved in this process (the liver). Once you grasp this concept, interpreting what hypoglycemia means and how to avoid it will become straightforward. Additionally, you need to consider proper recovery. As mentioned, frequent hypoglycemia can result from accumulated fatigue, leading to an overactivation of the nervous system.
In this post, we’ve broadly covered:
- The physiological meaning of hypoglycemia.
- Its potential impact on athletes.
- How it can compromise recovery.
- Ways to prevent it.
- The importance of understanding how your metabolism functions and how your glucose curve reacts to stimuli using Glucovibes.
References
- [1] Brooks GA. The precious few grams of glucose during exercise. Vol. 21, International Journal of Molecular Sciences. MDPI AG; 2020. p. 1–19.
- [2] Moore MC, Connolly CC, Cherrington AD. Autoregulation of hepatic glucose production. Vol. 138, European Journal of Endocrinology. BioScientifica Ltd.; 1998. p. 240–8.
- [3] Yang SW, Park KH, Zhou YJ. The Impact of Hypoglycemia on the Cardiovascular System: Physiology and Pathophysiology. Angiology. 2016;67(9):802–9.
- [4] Alghannam AF, Ghaith MM, Alhussain MH. Regulation of energy substrate metabolism in endurance exercise. Int J Environ Res Public Health. 2021;18(9).
- [5] Terink R, Witkamp RF, Hopman MTE, Siebelink E, Savelkoul HFJ, Mensink M. A 2 week cross-over intervention with a low carbohydrate, high fat diet compared to a high carbohydrate diet attenuates exercise-induced cortisol response, but not the reduction of exercise capacity, in recreational athletes. Nutrients. 2021;13(1):1–15.
