Do I have insulin resistance?

Hello Vibers! Today, we’re bringing you a new blog to clear up any doubts you might have about this trending topic: insulin resistance. What is it? Why does it occur? How can I identify it? What can I do? Keep reading to find all the answers to your questions.
Insulin resistance
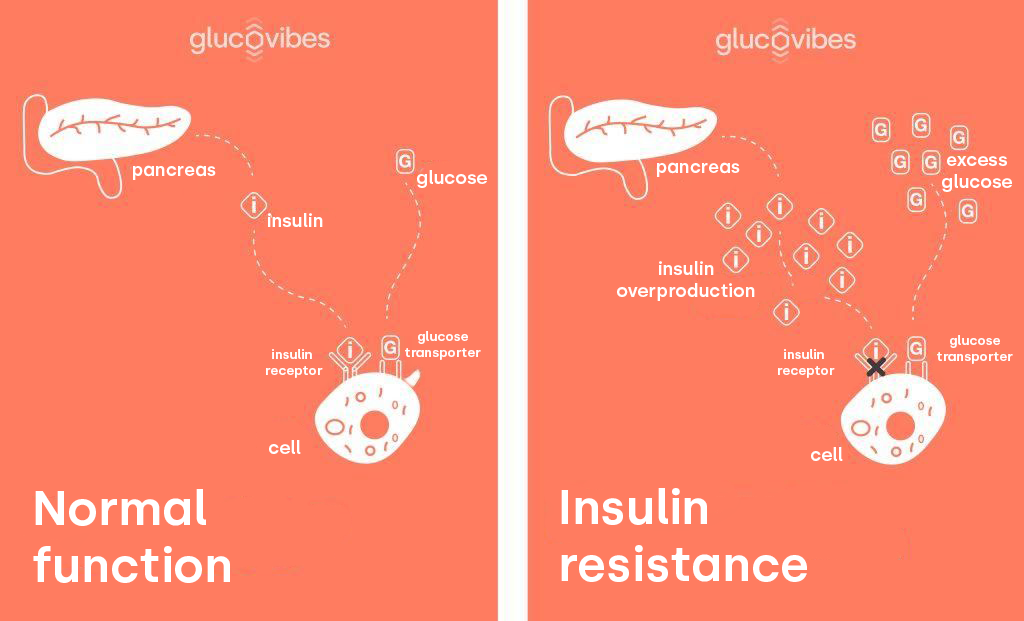
Insulin is a hormone secreted by the β cells of the pancreas in response to various stimuli, with glucose being the most relevant (1). Its main function is to maintain glucose homeostasis (the regulation of glucose levels) and other energy substrates. After each meal, insulin suppresses the release of free fatty acids while promoting the synthesis of triglycerides in adipose tissue (fat tissue). On the other hand, insulin inhibits the hepatic production of glucose (glucose production in the liver) while promoting glucose uptake by skeletal muscle and adipose tissue. In a state of insulin resistance (IR), the action of this hormone at the cellular level is reduced, leading to increased secretion to compensate and maintain glucose homeostasis (2). This phenomenon is characterized by hyperinsulinemia (excess insulin production), which is particularly evident in individuals with IR, especially after consuming a meal high in carbohydrates.
In epidemiological terms, the primary precursor of insulin resistance is the Westernization of lifestyle, defined by increased consumption of refined carbohydrates and plant-based unsaturated fats such as canola, soy, sunflower oils, and others, reduced physical activity, and chronic stress (3).
Although insulin resistance is a multifactorial process involving both genetic and acquired factors, there are several risk factors that can predispose an individual to develop this condition (4):
- Overweight
- Low physical activity
- Women with a waist measurement at the level of the navel exceeding 90 centimeters and men with a waist measurement over 100 centimeters
- Family history of type 2 diabetes
- Polycystic ovary syndrome
- Age over 45 years
- Blood pressure higher than 140/90 mmHg
- Low HDL cholesterol levels (35 mg/dl or less)
- High blood triglyceride levels (250 mg/dl or more)
Exercise/movement
Physical activity has a beneficial effect on insulin sensitivity in both normal populations and those with insulin resistance. It’s important to distinguish between the acute effects of exercise and the genuine effects of training. Up to two hours after exercise, glucose uptake is elevated partly due to insulin-independent mechanisms, likely due to an increase in the amount of GLUT4 associated with the plasma membrane and T-tubules induced by contraction. However, a single session of exercise can increase insulin sensitivity for at least 16 hours post-exercise. Consequently, recent studies have shown that acute exercise also enhances insulin-stimulated GLUT4 translocation. The increased GLUT4 protein content in muscle contributes to this effect, and it has also been hypothesized that the depletion of muscle glycogen reserves during exercise plays a role in this process.

Physical training enhances the effect of exercise on insulin sensitivity through multiple adaptations in glucose transport and metabolism. Additionally, training can lead to favorable changes in lipid metabolism and improve the regulation of glucose production in the liver, which is particularly important. Physical training plays an important, if not essential, role in the treatment and prevention of insulin resistance (5).
Nutrition
Given that the most important factor will be movement or physical activity, nutrition and diet are also crucial for improving insulin resistance. As mentioned earlier, reducing the intake of refined carbohydrates and unhealthy fats is key.
A Mediterranean diet, rich in vegetables and fruits, olive oil, and low-glycemic index foods, will be essential.
Here are some tips:
- Choose whole, unprocessed foods and avoid highly processed and prepared items.
- Opt for healthy unsaturated fats like nuts and seeds.
- Eat foods rich in fiber.
- Include vegetables in all your meals: they help control blood sugar levels.
- Consume fruits to get fiber, vitamins, and minerals, and avoid fruit juices.
- Include carbohydrates but in their whole form.
- Incorporate legumes as a source of carbohydrates.
- Include both white and blue fish in your diet.
- Add quality protein to your meals.
- Cook with olive oil.
Conclusions
Insulin is an anabolic hormone secreted by the β cells of the pancreas, and its main function is to maintain glucose homeostasis. In a state of insulin resistance (IR), the action of this hormone at the cellular level is reduced, leading to increased secretion to compensate and maintain glucose homeostasis. The primary precursor to insulin resistance is the Westernization of lifestyle, characterized by increased intake of refined carbohydrates and unsaturated fats from sources such as canola, soybean, and sunflower oils, along with reduced physical activity and chronic stress. Therefore, it is crucial to engage in physical exercise and maintain a healthy lifestyle with a balanced diet to ensure proper insulin function.
References
- [1] Fernando Carrasco N, José Eduardo Galgani F, Marcela Reyes J. Síndrome de resistencia a la insulina. estudio y manejo. Rev médica Clín Las Condes. 2013 ;24(5):827–37.
- [2] Galgani JE, Ravussin E. Postprandial whole-body glycolysis is similar in insulin-resistant and insulin-sensitive non-diabetic humans. Diabetologia. 2012; 55(3):737-42.
- [3] Kirk E, Reeds DN, Finck BN, Mayurranjan SM, Patterson BW, Klein S. Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Gastroenterology. 2009;136(5):1552-60.
- [4] Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, Zinman B; American Diabetes Association. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753-9.
- [5] Borghouts LB, Keizer HA. Exercise and insulin sensitivity: a review. Int J Sports Med. 2000;21(1):1-12.
